How We Can Fix This Pandemic in a Month
COVID19 - CORONAVIRUS, 12 Oct 2020
Damien Downing, MBBS, MRSB | Orthomolecular Medicine News Service - TRANSCEND Media Service
6 Oct 2020 – The Orthomolecular Medicine News Service has been publicizing the importance of vitamins D and C, and the minerals zinc and magnesium, in this pandemic since January [1]. I have been writing about vitamin D and sunlight for over 30 years [2], and it has never been more relevant.
If you caught the COVID19 virus right now, having a good vitamin D status (from already having taken a supplement) would greatly reduce your risk of contracting the infection, of the disease becoming severe, and of dying. Vitamin D enhances innate immunity while reducing the severity of inflammatory responses and supporting antioxidant activity [3]. Vitamin D deficiency correlates with risk of ARDS, sepsis and death from these [4]. You can even get some protection from living somewhere sunny [5] – or better still somewhere where people generally have good vitamin D status, probably from dietary sources [6].
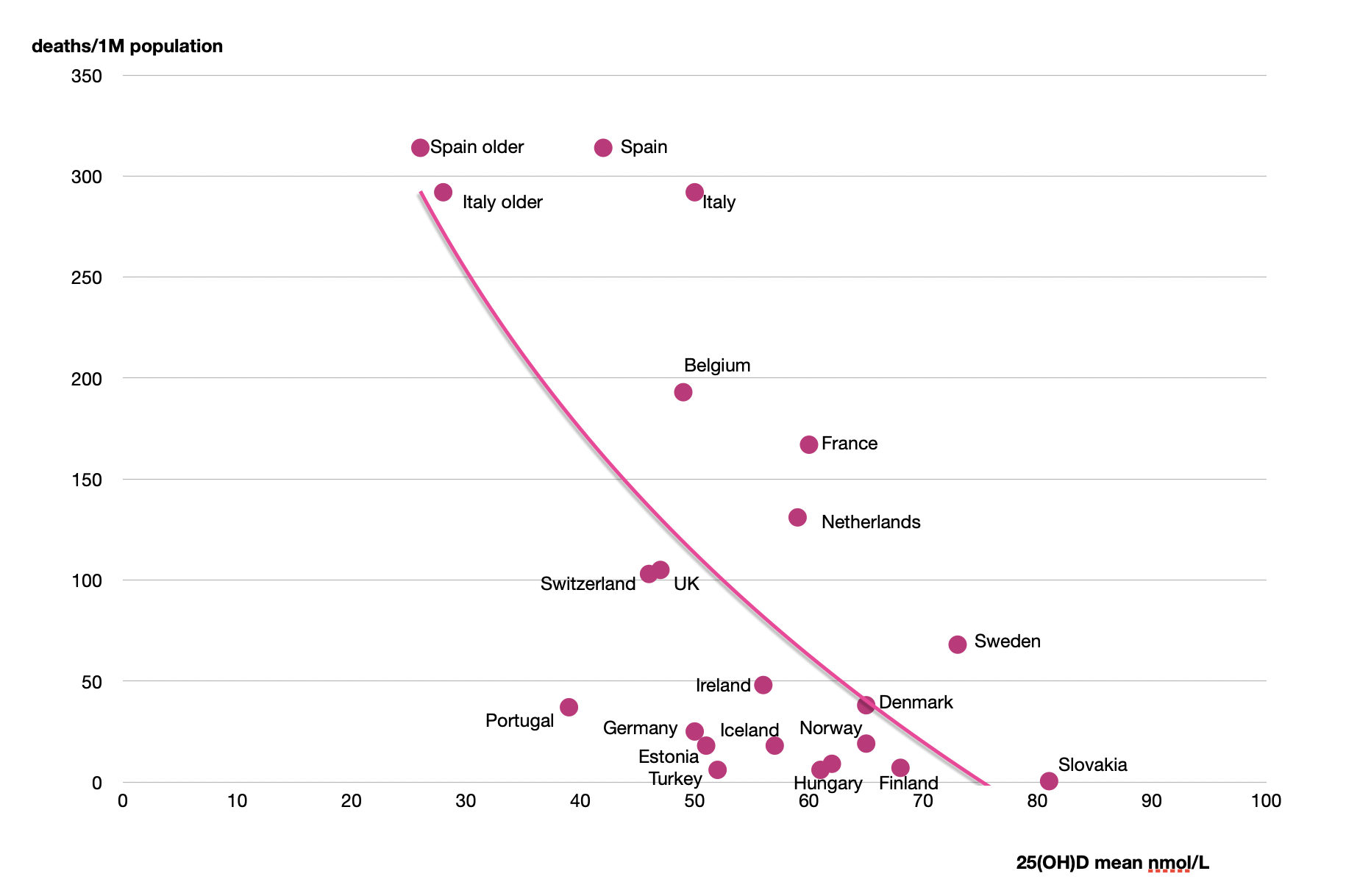
For countries in Europe, the probability of developing COVID-19, and of dying from it, is negatively correlated with mean population vitamin D status, with both probabilities reaching zero above about 75nmol/L, as clearly shown here [7]. The chart is redrawn from the original data, and also shows, at the top, the significantly lower vitamin D levels for the elderly in Spain and Italy.
Intervention!
We now also know that hitting the virus hard when you get infected can also work. Well, we already knew that vitamin C, zinc and magnesium worked (see any number of OMNS releases over the years). Recommended preventive adult doses are vitamin C, 3000 mg/day (in divided doses, to bowel tolerance), magnesium, 400 mg (in malate, citrate, or chloride form), zinc, 20 mg. [1]
What’s new is that vitamin D also works in the acute context. You want magic bullets? We got a handful now!
5 years ago a GP in Edmonton reported dramatic effects on influenza – “complete resolution of symptoms in 48 to 72 hours” from giving 50-60,000 IU of vitamin D3 [8]. Now a new study reports a similar effect on Covid-19.
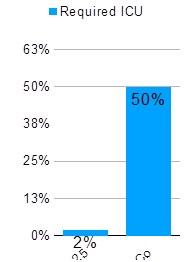
The new study, from Cordoba in Spain [9], looked at 76 patients admitted to hospital with signs of both Covid-19 and an acute respiratory infection. 26 patients had only the hospital’s standard care; 50 of them were given vitamin D as well. The form used was the 25-hydroxy D3, the more active form and the one that is usually measured in blood tests. The dose, given on days 1, 3 and 7, so over one week in effect, was equivalent to 128,000 IU in a week or 18,000 units every day of ordinary vitamin D3. This was a big dose, but not dangerous – see below.
What was the outcome? Here’s the graph. In the control group 50% of patients needed transfer to intensive care units; in the 25 (OH) D group only 2% – one patient out of 50.
Dosage is important and generally misunderstood
We have powerful tools here that could be employed right now to save lives; why are we not doing so? One reason is a widespread misunderstanding about dosage – of both vitamins D and C. In the UK this all seems to be down to one governmental committee.
The epidemiological paper cited above [7] shows that a vitamin D3 blood level of at least 75 nmol/L (30 ng/ml) is needed for protection against COVID-19. An adult will need to take 4000 IU/day of vitamin D3 for 3 months to reliably achieve a 75 nmol/L level [10]. Persons of color may need twice as much [11]. These doses can prevent, i.e. they can greatly reduce the risk of severe illness, but they are not enough for treatment of an acute viral infection – that takes the 60,000 to 120,000 IU dose acute intervention.
But governmental recommendations for vitamin D intake – 400 IU/day for the UK and 600 IU/day for the USA (800 IU for >70 years) and the EU – are based primarily on bone health and are woefully inadequate in the pandemic context. Several recently published papers have suggested that more than 4000 IU per day of vitamin D3 may carry a risk of harm, often citing the UK Scientific Advisory Committee on Nutrition (SACN) report of 2016 which set the recommended Upper Level (UL) intakes at 2000IU (50mcg) per day [12]. That report says; “Excessive vitamin D intakes have, however, been shown to have toxic effects (Vieth, 2006)”.
However this is misleading, as the 2006 Vieth paper [13] states: “Published reports suggest toxicity may occur with 25(OH)D concentrations beyond 500 nmol/L.” This leaves a wide margin of safety because 4000 IU per day will get you to about 75nmol/L – you would need to take more than 30,000 IU per day for three months to reach a 500 nmol/L blood level of vitamin D, to even run the risk of toxic effects.
What can we do?
If we had given everybody enough vitamin D six months ago when this all started – in March when the Northern hemisphere was not quite out of winter, and vitamin D levels were at their lowest – what would have happened? Well, I definitely believe that a couple of hundred black and Asian healthcare workers would still be alive (that’s just in the UK), along with a lot of people’s gramps and granmas who had to die alone in their care homes.
Two decades ago Richard Horton, editor of The Lancet wrote [14]; ‘When the state of the health of the people is at stake, we should be prepared to take action to diminish these risks even when the scientific knowledge is not conclusive.’ There is no good reason to wait for placebo-controlled trials to be conclusive here; we know that Vitamin D, vitamin C, zinc and magnesium will help and will do no harm.
So what would happen if we gave everybody enough vitamin D right now? In a population it would greatly reduce the risk of people contracting the infection, of the disease becoming severe, and of dying. Is that a 100% guarantee of your safety? Of course not, you’re not people; population studies can’t tell you about individuals – for a start they don’t know your vitamin D status now, or what else may be wrong with you.
For a government, though, it’s a far safer, and cheaper, bet than a vaccine that might never happen – you’d think. And the downside is negligible; if it simply didn’t work, we in the UK would have lost about what the Prime Minister just spent respraying his plane. And it would have made precisely nobody sick. The risk from not acting is much greater than the risk from acting.
Strike now
Strike now and we save lives. But I wouldn’t hold your breath until any of our governments takes appropriate action; you may have to do it yourself.
Michael Holick’s (he is one of the greats of vitamin D research) new app, D*minder, is a good place to start; it does a pretty good job on your D status, and its a free download. And buy some high strength vitamin D3 (no, fish won’t do it, and Cod Liver Oil has too much vitamin A).
Since our PM likes short pithy slogans, here’s one for all of us;
GET YOUR “D” UP!
Author’s note: I originally wrote this in June, basing the first part on two papers that were in pre-publication then. We have now been informed that the data in those two papers cannot be verified. We have no alternative but to withdraw that section. This release has now been rewritten to take account of that, and also of a new paper that considers vitamin D therapy in Coronavirus infection.
References:
1. Saul AW. (2020) Vitamin C Protects Against Coronavirus. Orthomolecular Medicine News Service. http://orthomolecular.org/resources/omns/v16n04.shtml
2. Downing D. (1988) Day Light Robbery. Arrow Books, London. ISBN-13: 978-0099567400
3. Grant WB, Lahore H, McDonnell SL, Baggerly CA, French CB, Aliano JA, Bhattoa HP. (2020). Evidence that vitamin D supplementation could reduce risk of influenza and COVID-19 infections and deaths. Nutrients, 12, 988. https://www.mdpi.com/2072-6643/12/4/988
4. Dancer, R. C. A., Parekh, D., Lax, S., et al (2015). Vitamin D deficiency contributes directly to the acute respiratory distress syndrome (ARDS). Thorax, 70(7), 617-624. https://doi.org/10.1136/thoraxjnl-2014-206680
5. Tang, L., Liu, M., Ren, B., Wu, Z., Yu, X., Peng, C., & Tian, J. (2020). Sunlight ultraviolet radiation dose is negatively correlated with the percent positive of SARS-CoV-2 and four others common human coronaviruses in the U.S. Science of The Total Environment, 751, 141816. https://doi.org/10.1016/j.scitotenv.2020.141816
6. Laird, E., Rhodes, J., & Kenny, R. (2020). Vitamin d and inflammation – potential implications for severity of COVID-19. Irish Medical Journal, 113:81-87. https://pubmed.ncbi.nlm.nih.gov/32603576 http://orthomolecular.org/resources/omns/v16n04.shtml
7. Ilie, P., Stefanescu, S., Smith, L. (2020) The role of Vitamin D in the prevention of Coronavirus Disease 2019 infection and mortality. Aging Clinical and Experimental Research, 32:1195-1198 https://link.springer.com/content/pdf/10.1007/s40520-020-01570-8.pdf
8. Schwalfenberg, G. (2015). Vitamin D for influenza. Canadian Family Physician, 61: 507. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4463890
9. Castillo, M. E., Entrenas Costa, L. M., Vaquero Barrios, J. M., Alcalá Díaz, J. F., Miranda, J. L., Bouillon, R., & Quesada Gomez, J. M. (2020). “Effect of Calcifediol Treatment and best Available Therapy versus best Available Therapy on Intensive Care Unit Admission and Mortality Among Patients Hospitalized for COVID-19: A Pilot Randomized Clinical study”. The Journal of Steroid Biochemistry and Molecular Biology, 105751. https://doi.org/10.1016/j.jsbmb.2020.105751
10. Vieth R, Chan PC, MacFarlane GD. (2001) Efficacy and safety of vitamin D(3) intake exceeding the lowest observed adverse effect level. Am J Clin Nutr, 73:288-294. https://pubmed.ncbi.nlm.nih.gov/11157326
11. Cashman KD, Ritz C, Adebayo FA, et al. (2019) Differences in the dietary requirement for vitamin D among Caucasian and East African women at Northern latitude. Eur J Nutr. 58:2281-2291. https://pubmed.ncbi.nlm.nih.gov/30022296
12. UK Scientific Advisory Committee on Nutrition (SACN) (2016) Vitamin D and Health. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/537616/SACN_Vitamin_D_and_Health_report.pdf
13. Vieth R (2006) Critique of the considerations for establishing the tolerable upper intake level for vitamin D: critical need for revision upwards. J Nutr, 136:1117-1122. https://pubmed.ncbi.nlm.nih.gov/16549491
14. Horton R. (1998) The new new public health of risk and radical engagement. Lancet. 352:251-252. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(05)60254-1/fulltext
______________________________________
 The peer-reviewed Orthomolecular Medicine News Service is a non-profit and non-commercial informational resource. Orthomolecular medicine uses safe, effective nutritional therapy to fight illness. For more information: http://www.orthomolecular.org. Comments and media contact: drsaul@doctoryourself.com
The peer-reviewed Orthomolecular Medicine News Service is a non-profit and non-commercial informational resource. Orthomolecular medicine uses safe, effective nutritional therapy to fight illness. For more information: http://www.orthomolecular.org. Comments and media contact: drsaul@doctoryourself.com
Go to Original – orthomolecular.org
Tags: Airborne contagion, COVID-19, China, Community, Compassion, Coronavirus, Cuba, Economy, Empathy, Environment, Health, Lockdown, Orthomolecular Medicine, PCR Tests, Pandemic, Public Health, Research, Science, Science and Medicine, Swiss Policy Research, United Nations, WHO
DISCLAIMER: The statements, views and opinions expressed in pieces republished here are solely those of the authors and do not necessarily represent those of TMS. In accordance with title 17 U.S.C. section 107, this material is distributed without profit to those who have expressed a prior interest in receiving the included information for research and educational purposes. TMS has no affiliation whatsoever with the originator of this article nor is TMS endorsed or sponsored by the originator. “GO TO ORIGINAL” links are provided as a convenience to our readers and allow for verification of authenticity. However, as originating pages are often updated by their originating host sites, the versions posted may not match the versions our readers view when clicking the “GO TO ORIGINAL” links. This site contains copyrighted material the use of which has not always been specifically authorized by the copyright owner. We are making such material available in our efforts to advance understanding of environmental, political, human rights, economic, democracy, scientific, and social justice issues, etc. We believe this constitutes a ‘fair use’ of any such copyrighted material as provided for in section 107 of the US Copyright Law. In accordance with Title 17 U.S.C. Section 107, the material on this site is distributed without profit to those who have expressed a prior interest in receiving the included information for research and educational purposes. For more information go to: http://www.law.cornell.edu/uscode/17/107.shtml. If you wish to use copyrighted material from this site for purposes of your own that go beyond ‘fair use’, you must obtain permission from the copyright owner.
Read more
Click here to go to the current weekly digest or pick another article:
COVID19 - CORONAVIRUS: