Africa’s Anti-Malaria Efforts Face a New Hurdle – Drug and Insecticide Resistance
AFRICA, 24 Apr 2017
Andrew Githeko – The Conversation
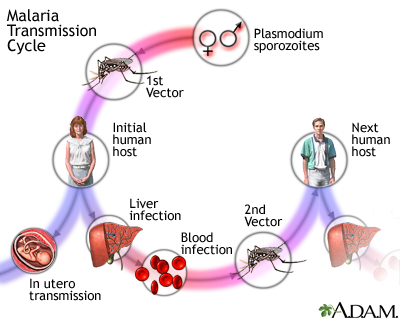
20 Apr 2017 – The resistance of malaria parasites to antimalarial drugs and insecticides is a growing global public health concern. The Conversation Africa’s Health and Medicine Editor Joy Wanja Muraya asked Dr Andrew Githeko to explain how African countries can maintain the effectiveness of existing malaria control strategies as they work towards its elimination.
The problem of drug resistant malaria is growing in Africa. The first case of resistance to the latest drug regimen was recorded in Equatorial Guinea two months ago. What does this mean?
There have been several more reports of drug resistance on the continent. Cases have cropped up in Angola, Liberia, Uganda and Equatorial Guinea. These show that there are serious challenges facing malaria treatment in Africa.
The main fear is that drug resistance in Africa will trigger the same intense transmission patterns that have been seen in South East Asia. The region has been battling drug resistance since 2007.
When mosquitoes become resistant to the insecticides this threatens to reverse the gains that have been made reducing the burden of malaria in endemic countries. By 2015, malaria interventions had reduced the prevalence by 50% and the incidence of clinical disease by 40%.
Africa has used the same treatment regimens that have been used across the world. This includes:
- chloroquine which was safe, cheap and effective until the malaria parasite –plasmodium falciparum– developed resistance towards it.
- sulphadoxine pyrimethamine a drug combination which also became resistant.
- artemisinin combination therapies which is the first line recommended malaria treatment which kills the parasites in the blood of the infected person within three days.
If resistance is developing to the artemisinin combination therapies on the continent, it means that the burden of the disease increases.
What unique challenges does Africa face in the fight against malaria?
The strategy to fight malaria in Africa includes antimalarial drugs and several other initiatives to prevent the mosquito from infecting people. The use of insecticide treated bednets and indoor spraying have been the most widely used.
These are all targeted at the malaria vector, the mosquito. But there are two challenges.
Firstly, mosquitoes have adopted survival tactics, changing their human biting behaviour and developing resistance to insecticides such as DDT and pyrethroid.
Before the widespread use of treated bednets, only 5% of mosquitoes were biting humans between 6pm and 9pm before people went to bed. Since bednets have been introduced, up to 15% of mosquitoes bite people before they go to bed, increasing the risk of infection.
Mosquitoes have also started to avoid resting on insecticide treated surfaces inside houses and instead bite and flee the house.
The second challenge is climate change which has resulted in mosquitoes breeding faster and the disease, in turn, spreading faster. Malaria is now present in areas that were previously not marked as transmission zones.
A third challenge faced in the urban environment is the lack of well managed drainage systems that would discourage mosquito breeding.
How can African countries tackle these challenges?
On the global front, the new combinations for malaria therapy must be urgently supported through a multilateral approach. This must involve the academia and governments and must be coordinated by the World Health Organisation.
At the national and regional levels, surveillance programmes should identify and document the spread of drug resistance.
In addition, new malaria control strategies should replace those that have lost efficacy. For example, chlorfenapyr is a pesticide that has been shown to be effective in India.
What is the way forward in the fight against malaria on the continent?
As a start it’s critical that the changing geographic distribution of malaria, which has been driven by climate change is mapped.
Malaria drugs should only be used where a correct diagnosis has been undertaken to reduce the misuse of malaria drugs and the cost of health care.
In addition, more attention should be paid to the architecture of houses in malaria endemic areas so that it prevents the entry of indoor biting mosquitoes. Research shows that when African rural houses are modified it can reduce the entry of mosquitoes by up to 80%. This strategy should be prioritised and adopted by national governments and local communities to reduce the risk of contracting malaria.
Governments should also increase and emphasise the use of treated bednets as a mosquito- repelling method targeting a coverage of 80%.
And lastly, an efficient drainage system should be introduced in malaria endemic areas. This can significantly reduce mosquito breeding habitats which will reduce the risk of malaria infections.
_________________________________
Andrew Githeko – Chief Research Officer, Kenya Medical Research Institute
Republish our articles for free, online or in print, under Creative Commons license.
Go to Original – theconversation.com
DISCLAIMER: The statements, views and opinions expressed in pieces republished here are solely those of the authors and do not necessarily represent those of TMS. In accordance with title 17 U.S.C. section 107, this material is distributed without profit to those who have expressed a prior interest in receiving the included information for research and educational purposes. TMS has no affiliation whatsoever with the originator of this article nor is TMS endorsed or sponsored by the originator. “GO TO ORIGINAL” links are provided as a convenience to our readers and allow for verification of authenticity. However, as originating pages are often updated by their originating host sites, the versions posted may not match the versions our readers view when clicking the “GO TO ORIGINAL” links. This site contains copyrighted material the use of which has not always been specifically authorized by the copyright owner. We are making such material available in our efforts to advance understanding of environmental, political, human rights, economic, democracy, scientific, and social justice issues, etc. We believe this constitutes a ‘fair use’ of any such copyrighted material as provided for in section 107 of the US Copyright Law. In accordance with Title 17 U.S.C. Section 107, the material on this site is distributed without profit to those who have expressed a prior interest in receiving the included information for research and educational purposes. For more information go to: http://www.law.cornell.edu/uscode/17/107.shtml. If you wish to use copyrighted material from this site for purposes of your own that go beyond ‘fair use’, you must obtain permission from the copyright owner.