Aedes Aegypti Mosquito: Fighting the Most Dangerous Animal in the World
HEALTH, 25 Jul 2016
Marian Blasberg, Hauke Goos and Veronika Hackenbroch – Der Spiegel
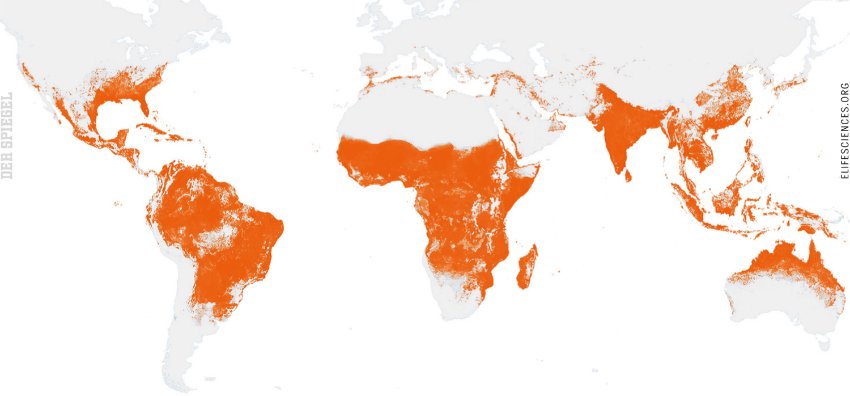
The Aedes aegypti mosquito, which carries Zika, dengue fever and other illnesses, appears unstoppable. It is posing a unique threat to this year’s Olympic Games in Rio and is rapidly spreading around the world. Europe, too, is at risk.

The Aedes aegypti has taken over the crown of the world’s most dangerous mosquito from the malaria-carrying Anopheles. The Aedes carries diseases such as dengue fever, yellow fever and Zika. Efforts are underway around the world to protect people from the Aedes aegypti and the diseases it transmits.
21 Jul 2016 – It is a Monday morning in April and a young man named Leandro Fornitan is heading into battle together with 300,000 male mosquitoes of the Aedes aegypti species. The insects are stored in several hundred plastic containers that have been loaded onto the bed of a truck Fornitan is driving through the streets of a residential district in the Brazilian city of Piracicaba. Aside from a few dogs, the streets are empty at this early hour.
The mosquitoes in the containers are 11 days old. And the deadly secret they are carrying with them is invisible.
Just like Aedes aegypti mosquitoes that grow up in the wild, Fornitan’s specimens have the same black-and-white striped pattern reminiscent of Adidas jogging suits. They all have the same bushy feelers, with which they navigate through their short lives — a life which, for a male Aedes, has but one aim: reproduction.
But the mosquitoes that Fornitan will release into the wild this morning were bred in a laboratory. And they possess an artificial genetic modification that will be passed on during mating. That gene produces a protein called tTAV, which will ensure that the mosquitoes’ larvae will die before reaching adulthood.
In other words, the genetically modified mosquitoes that Fornitan is currently testing in Piracicaba are manmade assassins being sent into battle against their own species. It is a kind of biological weapon, deployed with the goal of decimating the population of Aedes aegypti, a species that carries around a dozen diseases, many of them deadly, including yellow fever, dengue fever and other, largely unresearched illnesses such as chikungunya and Zika.
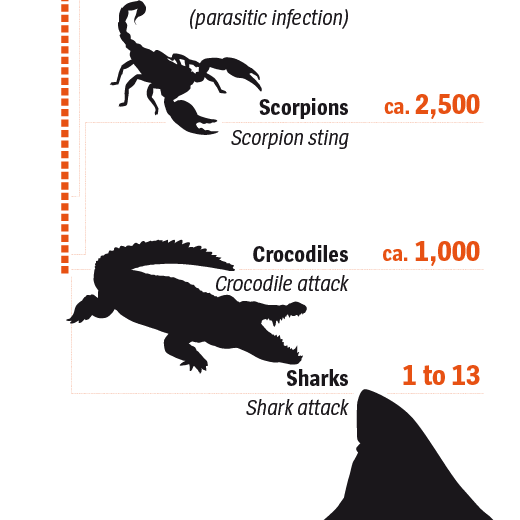
“This mosquito,” says Fornitan, “is the most dangerous animal in the world.” Indeed, Aedes aegypti presents a threat to some 4 billion people across the globe.
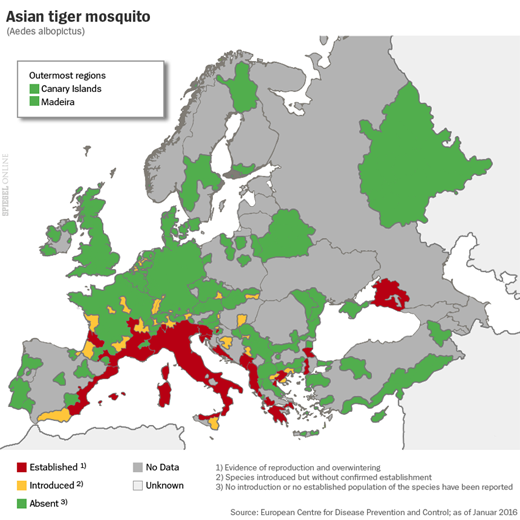
The world long approached the Aedes agypti plague as though it were a storm that would soon blow over, but it has now become a fixture in large cities in the tropics. If nothing is done, experts say, more and more people will die as a result. And it has also become clear that some of the tropical diseases carried by this insect are coming to Europe. Partly, that is the result of rising temperatures on the European continent. In the southwestern German city of Freiburg, for example, scientists have determined that a population of Aedes mosquitoes survived the German winter for the first time. It used to be that only those who traveled to the tropics were at risk of becoming infected with tropical illnesses. But now, many in Europe must face the prospect of the tropics coming to them.
It was images from Brazil that sent a jolt of fear around the world at the beginning of this year. Across the country, babies were suddenly being born with heads that were misshapen and too small. When indications mounted that this curious increase in cases of so-called microcephaly was connected to the Zika epidemic that had stormed across Brazil in the previous months, the World Health Organization (WHO) declared an international emergency.
The Mosquito of the 21st Century
Brazil mobilized 220,000 soldiers for the battle, sending them through bathrooms, yards and garages to eliminate standing water where female Aedes mosquitoes lay their eggs. But the campaign did little to reduce the threat. In the first four months of this year, officials registered 100,000 additional cases thought to be Zika. In addition, almost a million people were infected with dengue fever, more than ever before in such a short span of time.
There is no vaccine against the Zika virus and there is no medicine that can prevent people from becoming infected. In March, medical researchers said that Zika can also be transmitted via sexual intercourse and, as if that weren’t enough, 151 health experts wrote an open letter in May demanding that the Olympic Games — set to kick off in Rio in two weeks — be postponed or moved. Taking the risk of holding the games as planned, they said, would be irresponsible. The city is expecting a half-million visitors. If only a tiny fraction of them become infected by the virus, these games — intended to crown Brazil’s climb to economic power status — could mark the beginnings of a catastrophe.
The fear of a global Zika outbreak has put the spotlight on an insect that was long seen as the smaller, less dangerous brother of the Anopheles, which spreads malaria. But times are changing. Whereas the Anopheles was the mosquito of the 20th century, the Aedes aegypti seems intent on taking that crown for the 21st.
The number of people dying of malaria has long been in decline, but Aedes-spread dengue fever, by contrast, is now considered the fastest spreading mosquito-borne illness in the world. Fully 128 countries are now considered at risk of dengue and around 400 million people become infected each year, according to WHO. Most of them suffer from rashes, joint pain and high fever. But an estimated 20,000 per year have a different reaction: They experience severe internal bleeding which often ends in death.
It took dengue fever half a century before the WHO’s map of affected areas slowly turned red. But in the case of Zika, it is as though someone dumped a bucket of red paint on half the world. After the virus arrived in Brazil in 2013, likely by plane from French Polynesia, it only took a few months for it to spread to 60 countries. And everywhere Zika became established, it had been preceded by the Aedes aegypti mosquito.
The mosquito was also there when chikungunya fever broke out on the island of La Réunion in 2005. It was there when chikungunya spread to India and it was there when the virus jumped from the Caribbean to the American mainland. Even yellow fever, which long seemed to have been eradicated, is making a comeback. By the time Angola, the Democratic Republic of Congo and Uganda this spring reported the worst outbreak of the disease in decades, the mosquito had already infected 2,000 people. Three hundred of them died.

Aedes aegypti larvae inside an Oxitec laboratory in Campinas, Brazil. Oxitec has designed a genetic mutation passed along by male mosquitoes that causes larvae to die before reaching adulthood. Tests with the genetically modified insects have proven promising.
On the Front Lines
What, though, can be done? Will it be possible to eradicate the Aedes aegypti mosquito once and for all, or will we have to be satisfied with protecting ourselves to some degree from the diseases the insect carries?
The genetically modified laboratory mosquito from the British company Oxitec is the most innovative strategy yet developed to combat the insects. In trials on the Cayman Islands and in Panama, Fornitan says, their method succeeded in reducing the wild Aedes population by 90 percent in just a few months. They are now trying to do the same in Piracicaba.
Leandro Fornitan heads to the front lines six days a week. Next to him is an open laptop showing a map of the residential district. Whenever the computer peeps an alert, Fornitan reaches behind him, takes the lid off of one of the mosquito containers, holds it to a funnel sticking through his cracked window and pounds on the bottom of the container. A fan and the mosquitoes’ instincts do the rest.
“Normally,” Fornitan says, “we need one container every 100 meters. But there are hotspots where we release more” — such as scrap yards, bus stops and supermarkets.
The Aedes mosquito is never far from places where people live, work, play or wait. It is a problem facing Piracicaba and Rio de Janeiro, but also dozens of other cities worldwide, like Jakarta, Luanda and Singapore. They hide behind curtains, underneath beds and inside cars, constantly on the search for the scent of humans. Aedes aegypti is attracted both by the carbon dioxide that we exhale and by our perspiration, an alluring combination of butanoic acid and propanoic acid. Female mosquitoes pursue this scent until they come close enough to their victims to sense the warmth and dampness that everyone’s body emits.
In contrast to the Anopheles, which primarily bites at dusk and at night, Aedes aegypti females do most of their hunting during the daytime. You hardly notice when she caresses your skin with her feelers in the search for blood veins. The mosquito’s proboscis is made up of a lower lip and its six bristles. Some of the bristles have tiny hooks at their tips, which are drilled into the skin when the mosquito moves her head back and forth — until it finds a capillary to suck blood from.
Blood is vital for female mosquitoes. It provides the protein necessary to complete the egg creation process.
To prevent blood from quickly clotting, mosquitoes secrete an anticoagulant into their host’s bodies. It is this exchange of bodily fluids that makes mosquitoes into a so-called vector — an animal that transmits pathogens.
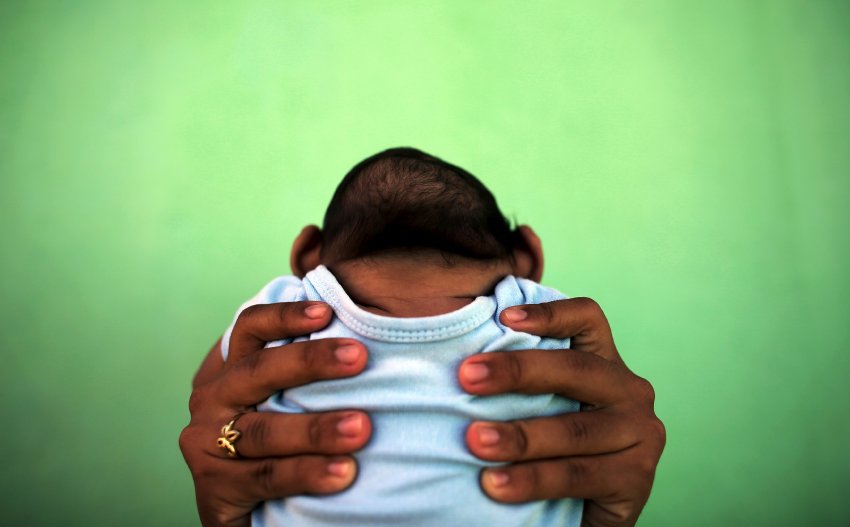
Zika has spread across Brazil in recent months, raising fears ahead of the Olympic Games, set to start in two weeks. An increase in the number of microcephaly cases, as seen in this image of a four-month old baby near Recife, Brazil, is apparently linked to the Zika virus.
Tricking the Mosquitoes’ Sense of Smell
As Oxitec’s genetically modified mosquitoes have become better known, demand has spiked. Last year, the US biotech firm Intrexon bought Oxitec — which was originally formed out of an Oxford University research project — for $160 million. Fornitan’s new bosses have practically lived in the air in recent months, traveling from hotspot to hotspot. Just in case their client’s desperation isn’t sufficient, they carry a study along with them that shows how significant the damage produced by the Aedes mosquito is.
In a country like India, the study notes, inpatient treatment of dengue fever patients can easily cost as much as half of a family’s annual income. In Thailand, the tourism industry estimates that dengue-induced revenue losses could amount to as much as $363 million. In Malaysia, researchers have calculated that 10,000 dengue cases resulted in the loss of 940,000 work days.
In order to do something about the Aedes, we need to have a clear understanding of the insect’s behavior. That is the common message delivered by those around the world who are trying to develop strategies to conquer the mosquito. James Logan agrees. A biologist at the London School of Hygiene & Tropical Medicine, Logan is one of just a handful of scientists around the world who is conducting research into how exactly mosquitoes behave.
Logan is searching for answers to fundamental questions. What are mosquitoes capable of perceiving? How do they find their victims? How have they managed to survive since the time of the dinosaurs?
“Mosquitoes were on this planet before us,” Logan says, “and most probably they will still be here when we have long gone.”
A Cocktail of Scent Molecules
Logan is an inquisitive 37-year-old who is unable to hide his admiration for the mosquito as he walks in his lab coat through the basement vaults where his institute’s insectarium is located. It is tropically humid in the room and the walls are lined with cages where Logan keeps the objects of his studies.
Logan reaches for a wired metal cylinder containing blood warmed to body temperature behind a transparent membrane. He sets the cylinder on one of the cages and within seconds, a swarm of mosquitoes flock to it. “Fascinating, isn’t it?” he says.
You have to look extremely closely to see on the mosquito’s head the two ultra-thin antennae it uses to navigate through its life. These antennae, which are equipped with thousands of receptors, are its most important organ. It is a kind of super sniffer that collects scents and leads the mosquito to standing water and to the human blood and plant nectar that it feeds on.
“Look at this room,” Logan says. “It looks quite empty. But for the mosquito, it is full of a cocktail of different odor molecules. We humans send out about 500 odor molecules, and the mosquito can detect about 20 of these. The CO2 of our breath, the carboxylic acid in our socks or the sweat on our skin. All this together tells the mosquito: Over there, there is a human.”
Logan believes that if we want to protect ourselves from mosquitoes, we have to outflank their sense of smell. That means that we have to change our bodily odors such that mosquitoes think: It’s not a human standing over there, but something else.
“Mosquito repellant,” Logan says, “is our first line of defense.”
For years, Logan has been testing the effectivity of such products for the pharmaceuticals industry, but it is challenging. DEET is still the most reliable substance out there, a synthetic molecule that was developed in the 1940s by the US military after it became clear that, in some wars, almost as many men were being lost to mosquitoes as to enemy fire. Logan explains that DEET activates certain receptors on the antennae, thus confusing mosquitoes. But DEET has two disadvantages. First, it has side-effects. And second, it doesn’t work as well on Aedes aegypti mosquitoes as it does on the Anopheles.
‘Constantly a Step Ahead’
Logan has thus resolved to take a closer look at the 10 percent of people whose blood, for as yet undetermined reasons, is ignored by mosquitoes — an attribute that is hereditary, as he has discovered. He found a number of such people and invited them into his laboratory for testing. He wrapped them in foil and siphoned off their bodily odors, which he then dissolved in a solvent and broke down into their component parts. He then connected the disembodied heads of dead mosquitoes (their antennae continue to function for up to an hour after death) to electrodes and passed the bodily odors over them, one component part after another. He then waited to see if his computers picked anything up.
He dreams of coming up with a remedy that will help normal people produce the natural anti-mosquito substance present in 10 percent of the population. A pharmaceutical company would then be able to produce a pill both for tourists and for those who are constantly threatened by the Aedes aegypti mosquito in their daily lives. But Logan isn’t sure how long it will take to develop such a drug. First, he says, the genes responsible for naturally producing the anti-mosquito substance must be identified. And even if he is successful, the question remains as to whether Aedes aegypti will become resistant to such a pill.
Like all mosquito researchers, he is well aware that Aedes aegypti has always had a response when humans have placed obstacles in its path. “Aedes is constantly a step ahead of us,” Logan says, “because it is able to adapt quickly.”
It is this flexibility in dealing with adversity that put humans on the mosquito menu in the first place. Back when mosquitoes lived exclusively in sub-Saharan Africa, they preferred targeting wild animals to sate their thirst for blood. Females mostly laid their eggs in branch hollows that filled with water during the rainy season. Evolution researchers have differing answers to the question as to when mosquitoes began changing their behavior. According to one theory, a changing climate was to blame. When the Sahara began expanding around 1,000 years ago, that meant that much of the mosquitoes’ habitat dried out, which in turn meant that water could only reliably be found in places where humans had settled — and these humans soon became their most stable source of blood.
A second theory holds that the domestication of the mosquito only happened much later, as a spontaneous event that took place on a slave ship traveling from Africa to the New World. That theory was developed by the Brazilian historian Rodrigo Magalhaes, who wrote his Ph.D. about the 20th century South American fight against an insect that has repeatedly caused yellow fever outbreaks since its arrival.
A Massive Effort in Vain
On a humid afternoon, Magalhaes is sitting in his bookstore in the heart of Rio. The temples of his eyeglasses are black-and-white striped, just like the body of the Aedes aegypti mosquito. Until the outbreak of Zika, he says, nobody was interested in his studies. Now, though, he is suddenly receiving a lot of attention.
Magalhaes refers to his research as “the astonishing story of a 100-years war,” one in which both sides, humans and mosquitoes have suffered devastating defeats. It is a story that makes clear the difficulties facing a researcher like Logan as he searches for a chemical substance that might ward off Aedes.
The tragic hero in Magalhaes’ drama is an American doctor named Fred Soper, who in 1947 became the coordinator of a program to eliminate the Aedes aegypti mosquito under the auspices of the Pan American Health Organization. It marked the first time that the world resolved to eliminate a vector in the effort to destroy a virus. And Soper believed that he possessed the miracle weapon that would make it possible: Dichlorodiphenyltrichloroethane.
DDT is a chemical whose potency as an insecticide was discovered in 1939 by an employee of the Swiss pharmaceutical company Geigy. Years later, he was awarded the Nobel prize for medicine.
Soper managed to get South American countries to change their laws such that local mosquito hunters were guaranteed access to private homes. For years, these teams traipsed through the streets of South American cities spraying DDT into living rooms, bathrooms and kitchens. They sprayed it on the fronts of buildings, on sidewalks and in public places — and in the countryside, airplanes sprayed the stuff on coffee and sugar plantations. Magalhaes says that for Aedes aegypti, the insecticide had the same effect that napalm did in Vietnam. They died on contact with DDT.
In 1958, 11 years after launching his campaign, Fred Soper announced that all countries in South and Central America had successfully eliminated the Aedes aegypti mosquito.
“The problem,” says Magalhaes, “was the United States.”
Resistance to DDT
Because the US hadn’t experienced a yellow fever epidemic since 1905 and because dengue and Zika hadn’t yet become a danger, American politicians were reluctant to spend millions of dollars to do battle against an apparently harmless insect. They ignored Soper’s entreaties.
By 1965, the Aedes aegypti was back, first in Mexico and then, one year later in Nicaragua and two years after than in the northern Brazilian city of Belém, where researchers determined that the mosquitoes had the exact same genetic code as Aedes aegypti mosquitoes in Florida.
Magalhaes leans back. “That the huge effort had been in vain was one problem,” he says. “The other was that Aedes aegypti was suddenly resistant to DDT.”
During the time when Soper’s army of sprayers was making its way through Central and South America, and perhaps even earlier, a change in the mosquito’s genetic code took place during one of the species’ myriad breeding cycles — one which made the insect immune to the poison. It was a mutation that guaranteed the survival of the species.
“It is a question of evolutionary intelligence,” says Magalhaes. Survival of the fittest.
Adapting to humans and the development of a resistance to DDT aren’t the only responses Aedes aegypti has found to its changing habitat. In contrast to the malaria-carrying mosquito Anopheles, Aedes was able to quickly adapt to conditions in rapidly growing megacities. Whereas they once bred in branch hollows found in the pre-historic African forest, today they are just as happy with car tires, plastic bottles or computer casings — the normal junk produced by tropical cities, left in the open to slowly decompose and to fill with water when it rains.
Aedes aegypti, the mosquito of the 21st century, has become established in the slums of cities like Rio de Janeiro, where the sewage system is just as dysfunctional as garbage disposal. In Piracicaba, the neighborhood mosquito hunters have found that the stomachs of many Aedes females can now hold twice as much blood as they could just 20 years ago. In a city like Singapore, which is lit up all night long, researchers have found that the mosquitoes now suck blood around the clock.
The forecasts of climate researchers also play into the hands of Aedes aegypti. Steady warming is one element, but more important is the possibility of an increasing number of droughts, which will lead more people to store water in vats on their rooftops.
The Search for a Vaccine
In Rio, the Secretariat for Tourism recently urged guests in town for the Olympic Games to avoid visiting favelas during their stay. In mid-June, shortly after the 151 scientists and doctors urged the cancellation of the games, a WHO emergency committee took a closer look at the situation in the city. The experts reached the conclusion that allowing the games to go forward would have little effect on the spread of the Zika virus, in part because the mosquito population had significantly shrunk during the cooler winter months.
But the committee, it would seem, has been unable to allay widespread fears. Recently, professional cyclist Tejay van Garderen, whose wife is expecting their first child, announced that he would not be participating in the games. Golfer Jason Day, the number-one ranked player in the world and a favorite for the gold, joined him. When the German track and field team recently cancelled a planned on-site training camp, there were complaints that there still isn’t a vaccine against the virus, despite its having been first identified 70 years ago in Uganda.
It is an understandable grievance. A vaccine for yellow fever was developed in the 1940s, but in the decades since then, there has been no additional vaccine created to protect humans from the diseases carried by Aedes aegypti.
Developing an injection that would render the mosquito harmless is a dream shared by Marie-José Quentin-Millet, who spent almost 20 years searching for a vaccine against dengue fever for the French company Sanofi Pasteur. “When we started,” she says, “we were all still young and beautiful!”
Quentin-Millet is standing in the visitors’ gallery of a snow-white factory building in the Lyon suburb of Neuville-sur-Saône. Behind a pane of glass, a biotech laboratory — with its gigantic bioreactors and dozens of pipes — can be seen, along with several lab workers sitting at their computers wearing surgical masks. She says she can hardly believe that a vaccine is now actually being produced.
“Dengue is so complex,” she says.
‘We Almost Gave Up’
The problem she faced in her efforts to conquer the virus is that there are four different varieties of dengue. In order to render all four of these so-called serotypes harmless, a four-in-one vaccine needed to be developed.
When Quentin-Miller and her team took up the challenge in the 1990s, they were like a group of mountain climbers trying to decide which flank would lead them most directly to the summit. They spent 10 years researching how they should start.
“There were moments,” Quentin-Miller says, “when we almost gave up.”
Ultimately, it was the well-established yellow fever vaccine that got them on the right track. They introduced two genes from each dengue fever serotype into the vaccine. Following promising tests on animals, they performed trials on small groups of people before finally performing large-scale studies involving the vaccination of 35,000 children in Asia and Latin America.
In the end, it wasn’t a single injection that rendered the mosquito harmless, but three, delivered at six-month intervals. Among the test subjects, the risk of becoming infected with dengue sank by 60 percent and the number of life-threatening cases sank by 80 percent. It wasn’t a perfect outcome, but better than nothing.
What, though, happens next? Over the years, Sanofi Pasteur invested 1.5 billion euros in the search for the vaccine — money that it, under the brand name Dengvaxia, must now recoup. In April, the first shipment left the factory and a short time later, 800 schoolchildren in the Philippines were vaccinated under the media spotlight. Mexican officials have also now approved Dengvaxia, as has Brazil.
But the Brazilian Health Ministry also announced in May that it was not going to include the vaccine in the country’s free public vaccination program. The ministry, it was reported, would have had to pay 22 euros for each dose. That is too much for a country that is currently trying to cut spending amid an economic crisis.
The Promise of Profit
Instead, newspapers reported, the vaccine was to be distributed via a network of private clinics, where a privileged minority can protect itself against the dengue virus for around 100 euros. The vast majority of the population, however, most of which lives in places where the mosquito has established itself, won’t be able to afford Dengvaxia.
Brazil is not a poor country, but it is a good example of the difficulties facing companies like Sanofi Pasteur in markets south of the equator. They must deal with governments that have tight budgets or a limited desire to invest in public health — or both. It is no accident that pharmaceutical companies in 2013 worked on the development of 183 medications for heart disease and only 18 for treating malaria. In contrast to health problems encountered in the industrialized world, tropical illnesses don’t hold the promise of profit.
That’s the good news for the mosquito. The bad news, though, is that the further it advances into wealthier countries, the greater the possibility that it will be targeted by pharmaceutical companies. Whereas Anopheles is primarily a problem for some of the poorest countries in Africa, the Aedes aegypti has crossed a red line. Countries like China and India have pulled out their calculators and are comparing the price of vaccines with the costs of treating dengue fever at public hospitals. That is the bet that Sanofi Pasteur has made — and it is one that others are making as well. Five additional dengue vaccines, it is said, are currently under development by companies around the world.
Sanofi Pasteur has also begun working on a Zika vaccine. The virus, says Quentin-Millet, is less complicated than the dengue virus. If scientists all work together, Quentin-Millet is convinced that it will take much less than 20 years to develop a Zika vaccine.
Still, it is an illusion to believe that a vaccine can completely conquer the mosquito. In fact, it is a fallacy that led countries like Angola, Congo and Uganda to believe that large-scale vaccination campaigns had brought an end to yellow fever. After the number of cases plunged dramatically in the 1980s, they gradually removed the illness from their vaccination programs. The result is that today, two generations later, yellow fever is back and in cities like Luanda, which the Aedes mosquito calls home, there is a shortage of the vaccine.
Indeed, it looks as though the battle against mosquito-borne illnesses is one that will continue for quite some time. Vaccines such as the one developed by Sanofi Pasteur might limit the risk of dying from a mosquito bite, but they don’t eliminate it — and neither do the mosquito repellants James Logan is testing in London. Everything that humans have thus far done to destroy the mosquito has failed in one way or the other. And Oxitec isn’t likely to change that. After six months, the number of dengue cases in the test region had sunk from 132 to just two and the Aedes aegypti population had shrunk by 90 percent. But that is about as much as can be expected, Fornitan says. The mosquitoes, he says, keep coming back — in cars, buses and trains.
A Volunteer Army
“The only thing remaining to us is vigilance and education,” says a small, wiry retiree named Justin Foo, who is waiting for two colleagues in front of a residential building in central Singapore. Foo used to work as an engineer, but today he wears the yellow vest of a “Dengue Prevention Volunteer.” He belongs to a kind of citizens’ militia that has joined the battle against the mosquito on behalf of state environmental authorities.
Foo points to a residential building that they are planning to visit. The inspectors used to find mosquito eggs in every second household in Singapore. Today, the ratio is 1:100.
Singapore is a small, densely populated country with 5.5 million inhabitants that lies almost exactly on the equator. That means that warm temperatures are constant and that rain falls at virtually the same time every afternoon, even outside of the rainy season. They were the kind of conditions perfect for the Aedes aegypti mosquito when soldiers and travelers unwittingly brought the species to Southeast Asia during World War II. Singapore experienced its first serious outbreak of dengue fever in the early 1960s. In 1966, the country established an authority to fight the disease and today, the Environmental Health Institute has 850 employees along with several thousand volunteers like Foo.
Over the decades, Singapore has developed a control system that is now seen as being unique in the world. It is a kind of mosquito secret police, which keeps a close eye on citizens and forces them to comply with regulations through a mixture of education and punishment.
The lifecycle of a female Aedes is at least 10 days long. During this period, they lay several hundred tiny eggs on four or five occasions. In contrast to the Anopheles, which lays its eggs on the surface of standing water, the Aedes mosquito positions its spawn just above the water’s surface. When the rain comes and the water level climbs, a new lifecycle begins in each egg.
Foo and volunteers like him are intent on breaking this cycle. It is his task to prevent the eggs from coming into contact with water.
At the health administration’s headquarters, all data relating to egg deposits are collected by computer and correlated with weather data, such as temperature, rainfall amount and how long the precipitation lasted. Individual finds are dismissed as being random, but if a second find is recorded in the same spot within 14 days, it is treated as a cluster, meaning that a public servant, known as a Vector Control Officer, is dispatched to spray the site with insecticide. If a resident wants to know if clusters have recently been found in his area or if there have been any recent cases of dengue, he can download a smartphone app that conveys such data.
Coming to Germany
In 2015, controllers undertook 1.4 million checks. On this morning, a routine patrol is on the schedule. As Foo and his colleagues walk through the residential block, they distribute brochures that tell residents what individuals can do in the battle against Aedes aegypti. The officers ring at every door and when it is opened, they smile amicably and take off their shoes before wandering inside. They shine their flashlights into toothbrush cups, turn over buckets stored under sinks and take a close look into flower pots on the balcony. If they find anything, residents must pay a fine equal to 130 euros. Repeat offenders pay another 130 euros and a third offense lands the offender in court.
Whereas soldiers in Brazil only went into action after a million people had become infected with the Zika virus, Foo patrols all year. Furthermore, the government of Singapore has pursued a clearly defined plan. The country invests around $2,000 per capita in the fight against the mosquito each fiscal year. Initially, after the program was introduced in the 1960s, the number of dengue cases plunged, before leveling off in the 1980s at around 9.3 cases per 100,000 residents.
Since then, though, the mosquitoes have retaken the city. Dengue washes over Singapore in waves, and if you look at the number of cases over the course of decades, it becomes apparent that the waves have become more frequent and the outbreaks more widespread. When the dengue-ratio climbed back over 300 cases per 100,000 in 2005, countermeasures were strengthened once again and a regular information campaign about disease outbreaks was reintroduced.
“It might sound absurd,” says a spokesperson at the Environmental Health Institute, “but the problems are a product of our success. The virus once again has an opportunity because our immune systems hardly produce antibodies anymore.”
Foo’s superiors now hope that the vaccine from Sanofi will soon be approved, even if it only offers limited protection against the dengue serotypes present in Singapore. Scientists are also campaigning for the deployment of the Oxitec mosquito — or they have proposed further experimentation with the Wolbachia mosquito, which are infected with bacteria that make them immune to dengue.
Bigger Gaps
There are dozens of strategies that humans are employing in the battle against the mosquito. But not a single one of them, it seems, has had the desired effect. It looks as though we will have to get used to the idea that mosquitoes will always find a gap in the safety net. And these gaps are getting bigger.
Thus far, Europe had thought it was safe. Viruses like dengue, Zika, and chikungunya, people thought, were largely a problem facing the developing world. When Germans became infected, it was generally those who had traveled to the tropics and not taken the warnings issued by the Foreign Ministry seriously enough. But it looks as though the rules of the game are slowly changing.
The German government is planning to provide 600 million euros in aid for vaccine campaigns by 2020 in the 22 poorest countries in the world — an initiative which, in times like these, could be interpreted as yet another substantial initiative to combat the root causes of flight. But that’s not all it is.
In 2010, southern France and Croatia registered the first autochthone cases of dengue fever in Europe since the 1920s, transmitted by mosquitoes living inside those countries, which means that the mosquito is getting closer and closer. In 2013, there was a dengue outbreak on the Portuguese island of Madeira with more than 1,000 cases.
“Aedes aegypti is essentially democratic. It doesn’t differentiate between the rich and poor,” says the biologist Norbert Becker, who has written several books about mosquitoes and spent the last 40 years fighting the insects on the upper Rhine River out of his office in Speyer. When he began his work in the summer of 1976, some people only left their homes in neoprene suits because they otherwise couldn’t stand the mosquito plague.
Becker smiles. “It used to be,” he says, “that the mosquitoes were just bothersome. Today, they are becoming increasingly dangerous.”
Researchers have verified the presence of five new mosquito species in Germany in the last 20 years, including two relatives of the Aedes aegypti that are capable of transmitting the same diseases: Aedes japonicas and the Asian tiger mosquito, Aedes albopictus.
‘Just a Question of Time’
Aedes albopictus, which likely came to Europe via Genoa, perhaps in a ship loaded with old tires that sailed in from America, was first identified in Germany at a highway rest stop near Weil am Rhein. In 2013, Becker counted six egg deposit sites. In 2014, he found 15 and by August of last year, 20.
In March, Becker then made an alarming discovery: Never before had an Aedes mosquito been discovered in Germany that early in the year. That could only mean one thing: The mosquito had apparently survived the German winter.
Becker leans back. “Essentially,” he says, “it was just a question of time.”
Becker has recently become part of a commission of experts that advises state governments, health ministries, city administrations and health authorities on what to do should the Asian tiger mosquito make an appearance.
Germany, it would seem, isn’t prepared for the mosquito. It isn’t enough to merely spray a few liters of insecticide in the area surrounding an egg deposit site. Aedes eggs can survive for an entire year without water. They are, if you will, violent, largely invisible sleeper cells and it doesn’t take much to activate them. A couple of warm days, a bit of water — the kinds of things that aren’t unusual in Rio de Janeiro, even in August.
Becker has dedicated four decades of research to the mosquito. He admires the creatures so much that he gave his daughter Daniela the middle name Aedes. In English, the word means ne’er-do-well.
DISCLAIMER: The statements, views and opinions expressed in pieces republished here are solely those of the authors and do not necessarily represent those of TMS. In accordance with title 17 U.S.C. section 107, this material is distributed without profit to those who have expressed a prior interest in receiving the included information for research and educational purposes. TMS has no affiliation whatsoever with the originator of this article nor is TMS endorsed or sponsored by the originator. “GO TO ORIGINAL” links are provided as a convenience to our readers and allow for verification of authenticity. However, as originating pages are often updated by their originating host sites, the versions posted may not match the versions our readers view when clicking the “GO TO ORIGINAL” links. This site contains copyrighted material the use of which has not always been specifically authorized by the copyright owner. We are making such material available in our efforts to advance understanding of environmental, political, human rights, economic, democracy, scientific, and social justice issues, etc. We believe this constitutes a ‘fair use’ of any such copyrighted material as provided for in section 107 of the US Copyright Law. In accordance with Title 17 U.S.C. Section 107, the material on this site is distributed without profit to those who have expressed a prior interest in receiving the included information for research and educational purposes. For more information go to: http://www.law.cornell.edu/uscode/17/107.shtml. If you wish to use copyrighted material from this site for purposes of your own that go beyond ‘fair use’, you must obtain permission from the copyright owner.